A pioneering study from the Newcastle Fertility Centre reports the first live births using pronuclear transfer, confirming the clinical viability of this technique to prevent the transmission of mitochondrial mutations in carrier women, under strict regulation and ethical monitoring.
In July 2025, The New England Journal of Medicine published the results of a groundbreaking study on the clinical application of mitochondrial donation through pronuclear transfer (PNT), a technique that enables women carrying mitochondrial DNA (mtDNA) mutations to have genetically related children with a significantly reduced risk of passing on severe diseases. The study, titled Mitochondrial Donation and Preimplantation Genetic Testing for mtDNA Disease, was led by a multidisciplinary team from the Newcastle Fertility Centre and the Wellcome Centre for Mitochondrial Research, in collaboration with other institutions in the UK and Australia. The findings mark a milestone in reproductive medicine and the prevention of incurable genetic diseases, showing that mitochondrial donation is compatible with embryo viability and can drastically reduce the burden of pathogenic mutations.
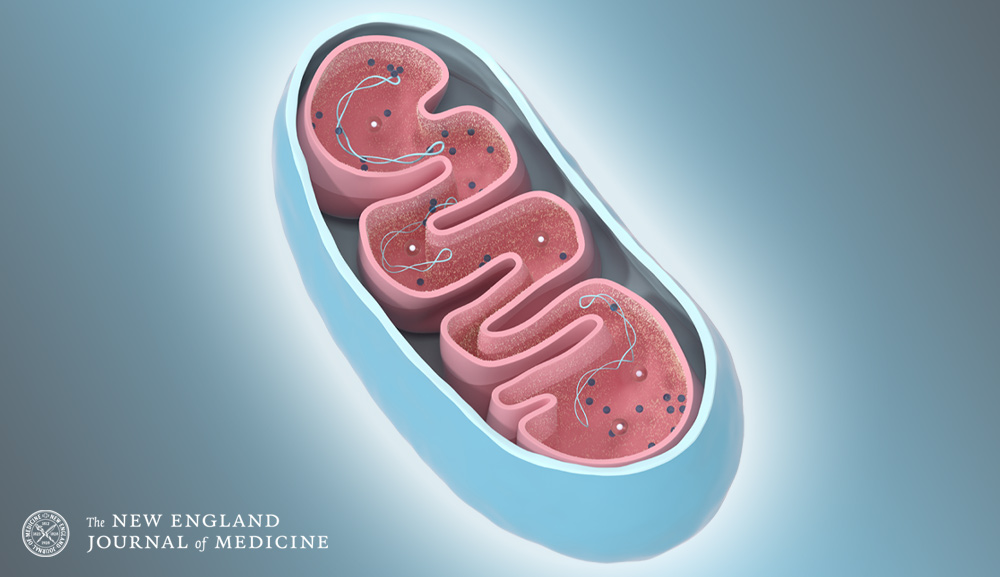
The research included 71 women carrying pathogenic mtDNA variants, who were treated using two complementary strategies: preimplantation genetic testing (PGT) for those with moderate levels of heteroplasmy, and pronuclear transfer for women with homoplasmic mutations or high levels of heteroplasmy. The latter technique involved removing the pronuclei (nuclear genetic material) from the patient’s zygote and transferring them into a donor egg that had been previously fertilized and from which the donor’s nuclear DNA had been removed. The result was an embryo containing the biological parents' nuclear DNA and healthy donor mitochondria, significantly lowering the inherited mtDNA mutation load.
The clinical outcomes are promising: eight live births were achieved through pronuclear transfer (four boys and four girls, including identical twins), and eighteen through PGT. Additionally, one woman treated with PNT was pregnant at the time of publication. Genetic analysis of blood samples from the babies born via PNT revealed a 77% to 100% reduction in mitochondrial mutation levels compared to the mothers' original values. In five of the eight babies, the mutation was undetectable, while in the remaining three, it was extremely low (5%, 12%, and 16%), levels considered safe and below the clinical threshold for disease development. All babies were meeting their age-appropriate developmental milestones—motor, cognitive, and social—and will be re-evaluated at age five to monitor for any late-onset complications.
The study, funded by NHS England and Wellcome, was approved by the UK’s Human Fertilisation and Embryology Authority (HFEA), which regulates the use of this technique under strict, case-by-case criteria. The clinical team included experts in embryology, genetics, reproductive biology, and mitochondrial medicine, such as Drs. Louise A. Hyslop, Mary Herbert, and Meenakshi Choudhary, and Professors Robert McFarland, Douglass M. Turnbull, and Robert W. Taylor, among other leading authors. All procedures were carried out in licensed facilities at the Newcastle upon Tyne Hospitals NHS Foundation Trust and under rigorous ethical oversight.
While the data suggest that PNT is less efficient than PGT in terms of implantation and pregnancy rates per embryo transfer, researchers emphasize that this technique remains a crucial option for women for whom PGT is not viable due to high mutation loads. In such cases, mitochondrial donation represents the only alternative to have genetically related children free from the hereditary burden of potentially fatal mitochondrial diseases. The authors also stress the need for long-term follow-up to better understand the stability of heteroplasmy levels over time and the possible effects of combining nuclear and mitochondrial genomes from different origins.
This study represents the first systematic clinical application of mitochondrial donation with birth follow-up worldwide, the result of over a decade of scientific development and legislative changes that began in 2015, when the UK Parliament approved the technique as part of reproductive medicine legislation. According to the authors, this is an effective strategy for reducing the risk of mitochondrial disease, though it should still be considered a risk-reduction measure rather than an absolute guarantee. As more countries and clinical centers consider adopting this technique, the work of the Newcastle team stands as a model of successful integration between basic research, bioethical regulation, and clinical application for the direct benefit of affected families.
Original article reference:
Hyslop, L. A., McFarland, R., Feeney, C., Turner, D., Herbert, M., … & Turnbull, D. M. (2025, July 16). Mitochondrial donation and preimplantation genetic testing for mtDNA disease. The New England Journal of Medicine. https://doi.org/10.1056/NEJMoa2415539
More information:
Centro Anáhuac de Desarrollo Estratégico en Bioética (CADEBI)
Dr. Alejandro Sánchez Guerrero
alejandro.sanchezg@anahuac.mx