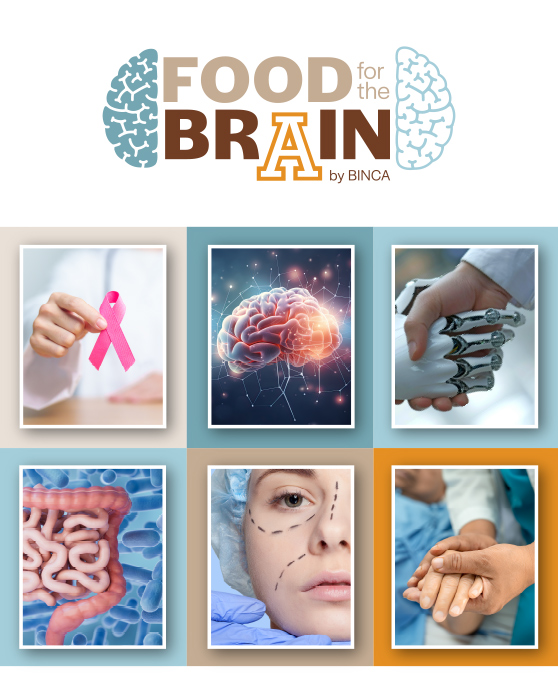
Specialists at BINCA analyzed the clinical, social and ethical challenges of composite vascularized tissue transplants, such as face transplants.
On January 28, 2026, BINCA, in collaboration with BeTrep, held a new academic session dedicated to reflection on transplantation in Mexico. The session featured the participation of Dr. Ernesto Cobos González and Dr. Ángel Uriel Cruz Reyes, who addressed medical advances, challenges, and the bioethical and social implications of vascularized composite tissue transplantation—particularly facial transplantation—from an interdisciplinary perspective grounded in the national context.
The session began with a statistical overview of transplantation in Mexico. Subsequently, Dr. Cobos introduced vascularized composite tissue transplantation, emphasizing its reconstructive purpose, the involvement of multiple tissues, and the process by which the graft is integrated into the recipient, thereby introducing the audience to the complex world of transplantation.
The discussion then turned to one of the most significant bioethical questions: life with a transplant versus life without one. Both positive and negative aspects were analyzed, highlighting the substantial risks faced by transplant recipients. The speaker emphasized that, due to immunological mechanisms secondary to the chronic treatments these patients must undergo, they become susceptible to rejection, severe opportunistic infections, cancer, metabolic alterations, among other important risks that must be carefully evaluated.
Nevertheless, the other side of the issue was illustrated through real patient cases in which individuals, after regaining limbs or other parts of the body, experienced a marked improvement in their quality of life.
This led to the introduction of a novel topic: the discussion of social death, understood as the isolation, stigmatization, loss of identity, deterioration of social roles, and disfigurement experienced by some candidates for complex transplants. From this perspective, transplantation seeks not only to restore an anatomical function but also to open the possibility of reconstructing the patient’s social life, although without fully guaranteeing it.
The bioethical analysis further explored informed consent, underscoring that in this type of procedure, patients can hardly provide fully informed consent due to technical complexity, uncertainty of outcomes, and external pressures—familial, social, cultural, and even medical—that influence decision-making. It was emphasized that accepting such a transplant entails recognizing the absence of satisfactory therapeutic alternatives and assuming long-term physical, psychological, and social consequences.
Likewise, reflection was offered on the specific challenges of the Mexican context, where transplant programs face structural limitations, emerging ethical dilemmas, and the need for highly specialized and multidisciplinary teams capable not only of performing surgery but also of supporting patients through selection, follow-up, decision-making, and transparent communication of risks and benefits.
The session concluded with a critical reflection on the true scope of contemporary medicine: the technical ability to reconstruct the body does not always equate to the ability to reconstruct life. In this sense, the importance of strengthening bioethical analysis, interdisciplinary collaboration, and institutional responsibility was emphasized to ensure that transplants are carried out with an approach centered on dignity, identity, and the comprehensive well-being of the patient. In addition, Dr. Cobos and Dr. Cruz extended an invitation to the BINCA community to apply to BeTrep’s research lines focused on transplantation.
BINCA
More information:
Clinical Bioethics and Neuroethics Anáhuac (BINCA)
Dra. María Fernanda Martínez Palomo
neuroetica@anahuac.mx